Non-celiac Disease: When Symptoms Are Real, but the Culprit Isn’t Gluten!
I have seen first hand the distress that symptoms without a diagnosis can cause. Honestly, it is just as agonizing for a healthcare professional as it is for the patient. We like a diagnosis for a symptom because it gives us a target to aim therapy at, with the happy outcome of helping someone feel better. And, truthfully, it makes us feel like we accomplished something. For the patient, it offers affirmation: “My symptoms are real. I have a diagnosis!” It provides recognition that what they are feeling is valid and understood.
This is why nearly 10% of our population has formed such a deep attachment to the diagnosis of “gluten sensitivity.”(1) The symptoms, abdominal pain, bloating, brain fog, fatigue, are real physical symptoms. No argument there. But the culprit, gluten, has been mistakenly blamed, and this misunderstanding has come with serious consequences: unnecessary fear around food, higher food costs, increased risk for heart disease, metabolic health problems, loss of whole-grain nutrients that protect long-term well-being, and possible increased risk of lower-gut disease. (2, 3, 4) All of this, layered on top of the anxiety that restrictive eating patterns can create, is amplified by an industry that profits from confusion and fear. (1, 2, 3)
Such entrenched attachments are hard to overcome. But the science is clear.
The physical symptoms are real.
Gluten is not the culprit.
The consequences of misdiagnosis are significant.
Here is the evidence:
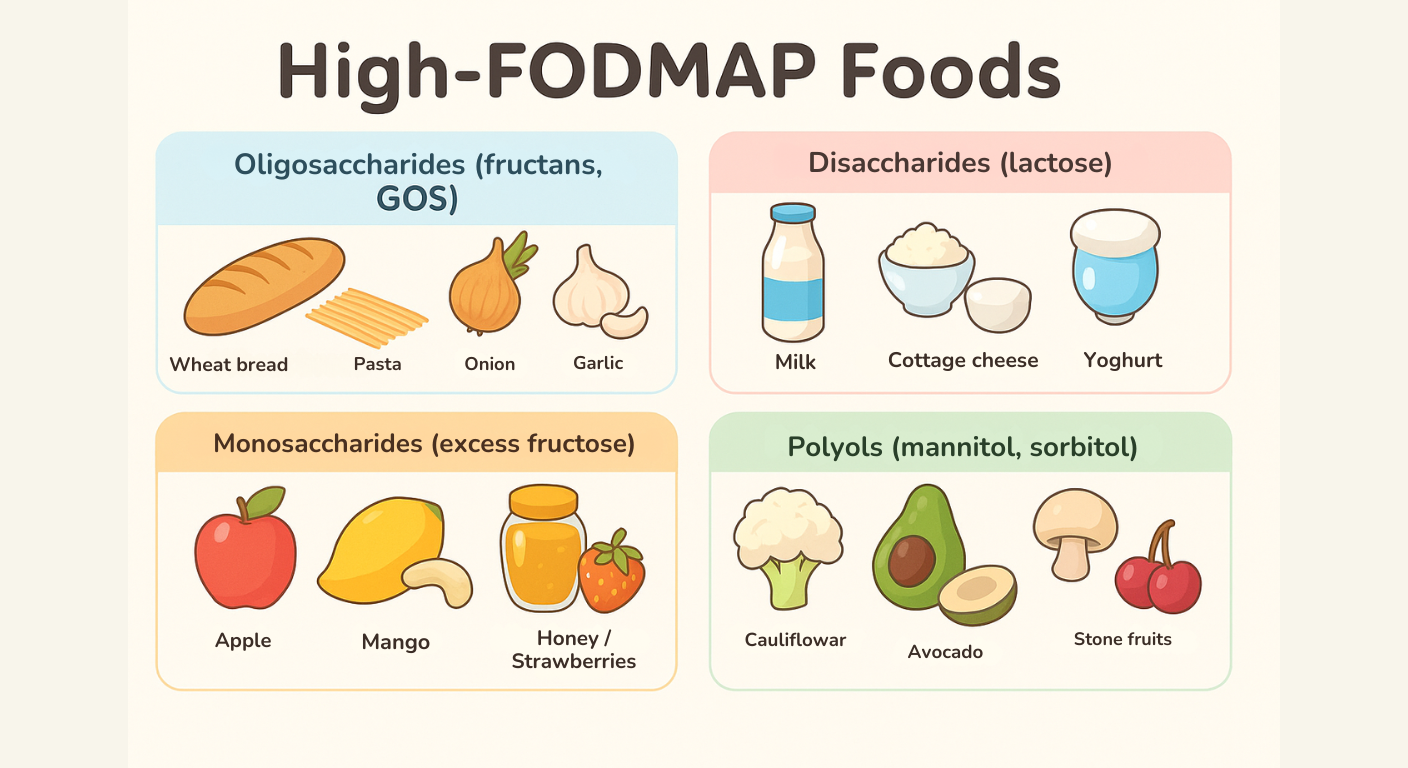
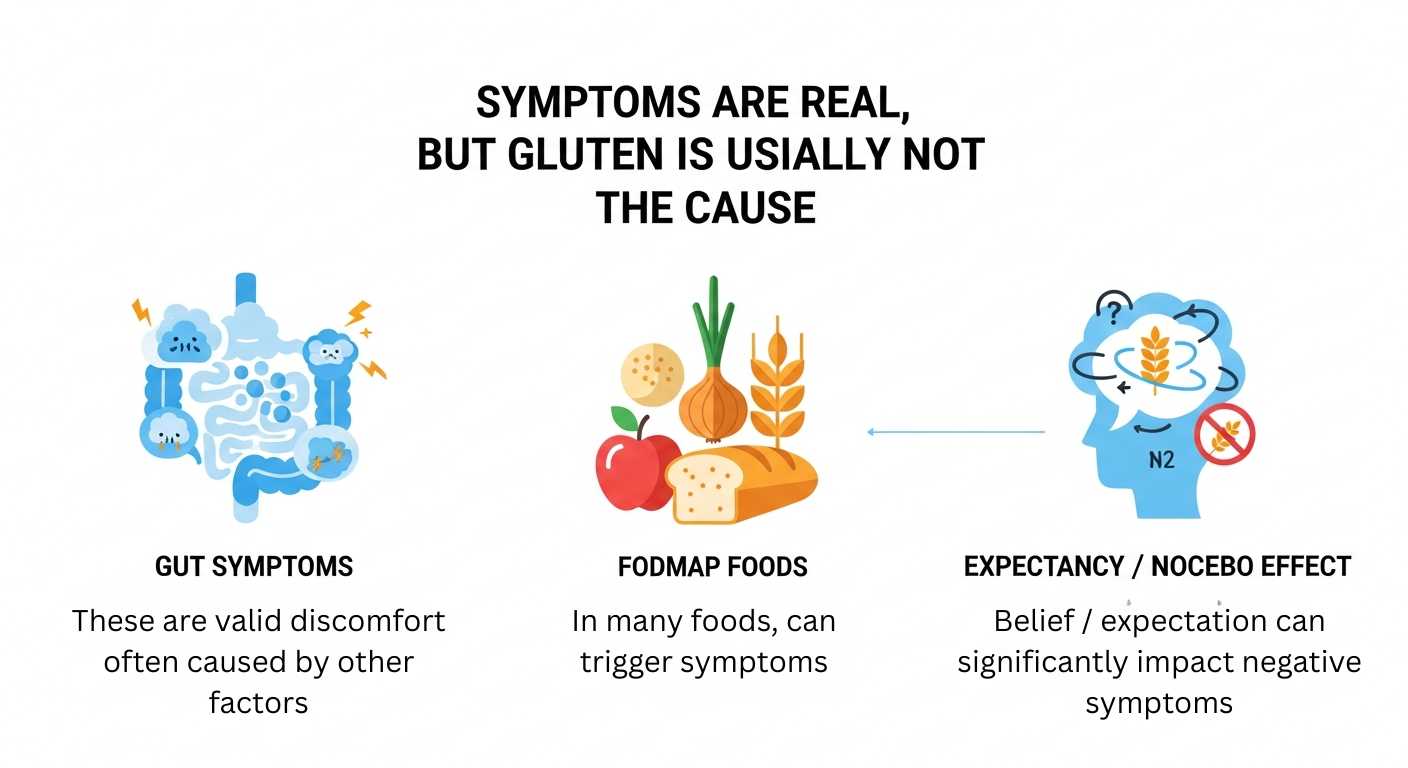
Drawing on large double-blind clinical trials and reviews (1, 2, 3, 4), brain-imaging research (5), and immunologic studies (4), we now know that for people without a diagnosis of celiac disease, gluten itself is rarely the cause of these symptoms. In double-blind studies where participants do not know whether they are consuming gluten or a placebo, they experience the same level of pain, bloating, fatigue, or brain fog in both conditions. This means that the symptoms are real! But the trigger is not gluten! Instead, the causes are more likely other food components such as FODMAPs (particularly fructans found in many everyday foods), and/or the brain's threat-response system, known as the nocebo effect, which activates even before food is eaten. (1)
In contrast, true gluten injury occurs only in celiac disease, an autoimmune condition affecting about 1% of the population, in which gluten attacks the small intestine and strict lifelong avoidance is essential.
The concern is significant with dire medical consequences: when people remove gluten without a medical diagnosis, they remove healthy whole grains that supply the balance of fiber, folate, iron, and other critical nutrients, nutrients delivered with natural elements that increase uptake and utilization of the essentials. Research has shown that over time this will increase long-term cardiovascular risk, reduce microbial diversity in the gut, disrupt balanced nutrition/absorption, and contribute to chronic anxiety/hypervigilance around eating — all while needlessly dramatically increasing food costs. (1, 2)
So yes — the suffering is real. But blaming gluten keeps people stuck, suffering, and afraid of food, instead of moving toward the real causes and real solutions that can help them feel well again.
Direction from the literature:
deGraff, et al., demonstrated that expectancy (i.e. believing one consumes gluten) plays a major role in triggering gastrointestinal and extra-intestinal symptoms, showing strong nocebo effect in NCGS/NCWS. (1)
Croall, et al., identified that when using imaging to explore neurological symptoms in self-reported NCGS (so-called “brain fog”). While small and preliminary, this identified the measurable brain changes associated with anticipating gluten/wheat-sensitivity symptoms. (5)
A review of the literature by Salmela, et al., found in their review of all double-blind, placebo-controlled gluten challenge trials in individuals without celiac disease, that only a small fraction had gluten-specific reactions, highlighting that most self-reported “gluten sensitivity” lacks objective confirmation. They identified symptoms are real. The link to gluten is not. (2, 3, 4)
The long-term gluten-challenge/ placebo-controlled trials show that only a small minority of self-reported gluten-sensitive people have reproducible reactions to gluten, meaning for most, gluten per se is unlikely the culprit! (3)
The recent reviews (2025) reflect the scientific community’s uncertainty: there is still no biomarker for NCGS/NCWS, and diagnosis remains by exclusion. This makes self-diagnosis and long-term gluten-free diets risky. (6)
Notable Quotes:
“The combination of expectancy and actual gluten intake had the largest effect on gastrointestinal symptoms, reflecting a nocebo effect.” (1)
“The majority of patients with suspected NCGS are not able to identify when challenged with gluten in a double-blind placebo-controlled food challenge, indicating that gluten is not the cause of their symptoms.” (2)
Reference:
de Graaf MCG, Lawton CL, Croden F, Smolinska A, Winkens B, Hesselink MAM, van Rooy G, Weegels PL, Shewry PR, Houghton LA, Witteman BJM, Keszthelyi D, Brouns FJPH, Dye L, Jonkers DMAE. The effect of expectancy versus actual gluten intake on gastrointestinal and extra-intestinal symptoms in non-coeliac gluten sensitivity: a randomised, double-blind, placebo-controlled, international, multicentre study. Lancet Gastroenterol Hepatol. 2024 Feb;9(2):110-123. doi: 10.1016/S2468-1253(23)00317-5. Epub 2023 Nov 28. Erratum in: Lancet Gastroenterol Hepatol. 2024 Mar;9(3):e8. doi: 10.1016/S2468-1253(24)00014-1. PMID: 38040019. https://pubmed.ncbi.nlm.nih.gov/38040019/
Dale HF, Hatlebakk JG, Hovdenak N, Ystad SO, Lied GA. The effect of a controlled gluten challenge in a group of patients with suspected non-coeliac gluten sensitivity: A randomized, double-blind placebo-controlled challenge. Neurogastroenterol Motil. 2018 Mar 15. doi: 10.1111/nmo.13332. Epub ahead of print. PMID: 29542844. https://pubmed.ncbi.nlm.nih.gov/29542844/
Salmela E, Kalle K, Lindfors K, Saavalainen P, Huhtala H, Kaukinen K, Taavela J. Long-term health outcomes of people without celiac disease avoiding gluten consumption: a 25-year prospective cohort study. Eur J Clin Nutr. 2025 Oct;79(10):1053-1059. doi: 10.1038/s41430-025-01641-x. Epub 2025 Jul 8. PMID: 40629072; PMCID: PMC12537484. https://pmc.ncbi.nlm.nih.gov/articles/PMC12537484/
Molina-Infante J, Carroccio A. Suspected Nonceliac Gluten Sensitivity Confirmed in Few Patients After Gluten Challenge in Double-Blind, Placebo-Controlled Trials. Clin Gastroenterol Hepatol. 2017 Mar;15(3):339-348. doi: 10.1016/j.cgh.2016.08.007. Epub 2016 Aug 12. PMID: 27523634. https://pubmed.ncbi.nlm.nih.gov/27523634/
Croall ID, Hoggard N, Aziz I, Hadjivassiliou M, Sanders DS. Brain fog and non-coeliac gluten sensitivity: Proof of concept brain MRI pilot study. PLoS One. 2020 Aug 28;15(8):e0238283. doi: 10.1371/journal.pone.0238283. PMID: 32857796; PMCID: PMC7454984. https://pubmed.ncbi.nlm.nih.gov/38040019/
Manza, F., Lungaro, L., Costanzini, A., Caputo, F., Carroccio, A., Mansueto, P., Seidita, A., Raju, S. A., Volta, U., De Giorgio, R., Sanders, D. S., & Caio, G. (2025). Non-Celiac Gluten/Wheat Sensitivity—State of the Art: A Five-Year Narrative Review. Nutrients, 17(2), 220. https://doi.org/10.3390/nu17020220. https://www.mdpi.com/2072-6643/17/2/220?utm_source=chatgpt.com